New Research Examines Antibiotic Resistance in Gonorrhea in Kenya
About the research
Across the globe, rates of sexually transmitted infections are on the rise, including gonorrhea. At the same time, the antibiotics usually used to treat gonorrhea are decreasing in effectiveness due to multidrug resistance.
Supriya Mehta, PhD, interim dean of global health and professor of epidemiology at the University of Illinois at Chicago (UIC) School of Public Health, is leading a project funded by the U.S. Department of Defense Global Emerging Infections Surveillance program to study antibiotic resistance in gonorrhea in people living in Kisumu, the third-largest city in Kenya.
“This is a global problem, and the challenge is you can’t take results from one area and copy them over to another area,” Mehta said. “Many countries have treatment guidelines for gonorrhea, but they need to be specific to local epidemiology and local microbiology.”
In Kisumu, from 2000 to 2010, resistance to ciprofloxacin, a fluoroquinolone drug that was commonly used to treat gonorrhea, grew from zero percent of gonorrhea samples to 50 percent of gonorrhea samples. In 2015, the Kenyan government updated guidelines for antibiotic therapy for gonorrhea, to switch from fluoroquinolones to cephalosporins, and Mehta’s research was part of this decision-making. In research Mehta led and published in 2020 in the International Journal of STD and AIDS, new study found that 100 percent of gonorrhea samples were resistant to fluoroquinolones. Additionally, 100 percent of gonorrhea samples were resistant to penicillin and tetracycline. These data show that resistance is driven by high rates of antibiotic use, not just for gonorrhea but for other types of infections as well.
Combatting this resistance is particularly important due to the effects of gonorrhea left untreated. In women, the infection can cause infertility and ectopic pregnancies, and in pregnant women, the infection can be transmitted to fetuses. Among both men and women, gonorrhea can increase rates of HIV transmission and acquisition.
Story, continued
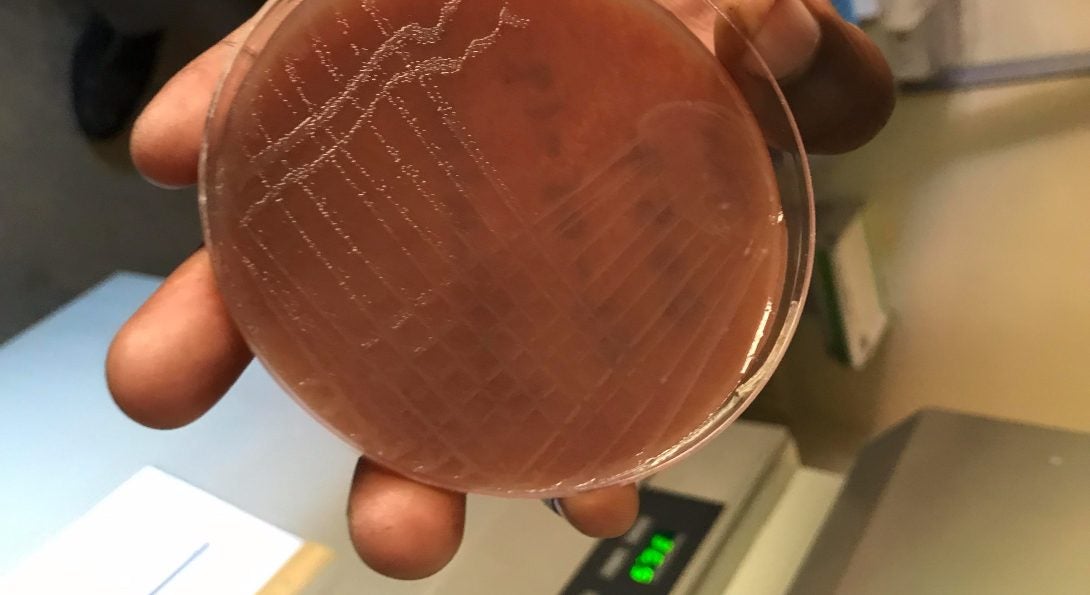
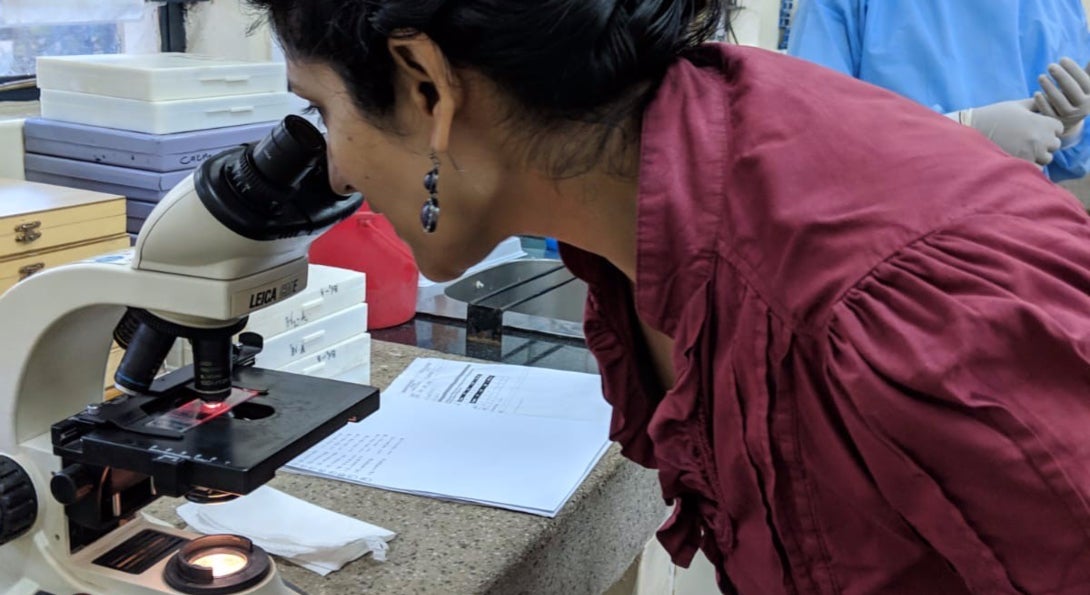
Mehta traveled to Kisumu in January 2020 to implement a new study of antibiotic resistance surveillance in gonorrhea. She led training on standardizing the collection and recording of data and observed the beginning of the study, observing how staff recruited and gained consent from participants, obtained medical histories and collected samples, and completed the process of laboratory testing. Results of this study can help inform the Kenyan government’s guidelines toward antibiotic therapy.
“We’re looking to identify individual-level factors associated with drug resistance,” Mehta said. “Are these older or younger men, those with multiple sex partners, or people coming from certain geographic locations? When we know where emerging resistance is coming from, we can carry out more intensive intervention and screening,” Mehta said. “Looking at these patterns globally, we hope to find emerging trends over time and geographic patterns.”
Mehta works with the Chicago Department of Public Health to conducting similar surveillance in Chicago. Since 2010, the United States, the Centers for Disease Control and Prevention (CDC) recommends dual antibiotic therapy for gonorrhea. In partnership with Chicago Department of Public Health, Mehta studied how healthcare providers in the city adhered to the new guidelines, finding that provider adherence to treatment guidelines improved over time, but still has room for improvement for female patients, and patients in non-specialist clinical settings. Former students Sara Stokes, MPH in Epidemiology ’19, and Christine Fukuda, MPH in Epidemiology ’19, also worked on enhanced gonorrhea surveillance and presented findings at the national CDC STD Prevention Conference in 2019.
“Even though we can’t take results from one area and copy them over to another area, we can translate and adapt our tools for studying gonorrhea to generate globally connected data,” Mehta said.