How Simulations Developed Illinois’ COVID Response
The Illinois Preparedness and Emergency Response Learning Center worked with public health agencies to prepare for disasters of all types.
Soldier Field’s parking lot is full. A long line of Chicagoans snakes out the entrances to the stadium. Television news reporters broadcast live on site. Traffic is backed up on Lake Shore Drive as people head to the field.
This scene is a familiar sight to football fans, except it’s not an ordinary football Sunday. On the turf, doctors and nurses are administering vaccines, one after another, to combat a new infectious disease.
That might sound like a snapshot of the future as Chicago and Illinois grapple with COVID-19, but it’s actually a slice of the past. The exercise in mass vaccination was one of a myriad of public health preparation projects led by the Illinois Preparedness and Emergency Response Learning Center at the University of Illinois at Chicago (UIC) School of Public Health, a Centers for Disease Control and Prevention-funded program from 2010-2015. The Center, which began as the Illinois Public Health Preparedness Center (funded from 2000-2010), worked closely with the Illinois Department of Public Health, Chicago Department of Public Health and Cook County Department of Public Health to enhance the capacity and performance of the public health workforce to prepare for and respond to man-made and natural disasters. Guddi Kapadia, assistant director of the Policy, Practice and Prevention Research Center at the School of Public Health, led the Center’s efforts.
Selected Quote
The Center was a huge win for public health. This funding linked academic expertise to state and local health agency need around preparedness education.
| Assistant Director, Policy, Practice and Prevention Research Center
Story, continued

While the COVID-19 outbreak is an unprecedented situation in modern times, the Center’s past pandemic preparedness trainings with the city and state helped lay the groundwork for today’s response. In 2009, Kapadia led trainings on H1N1, building awareness and mitigation strategies for public health practitioners and healthcare delivery workers.
“We heard that when a newer virus becomes identify, it seems that we forget all the basics about universal precautions,” Kapadia said. “We were engaged in many of the same practices in 2009 as we are now, it was the three C’s that we were sharing then – clean, cover and contain, sound familiar?”
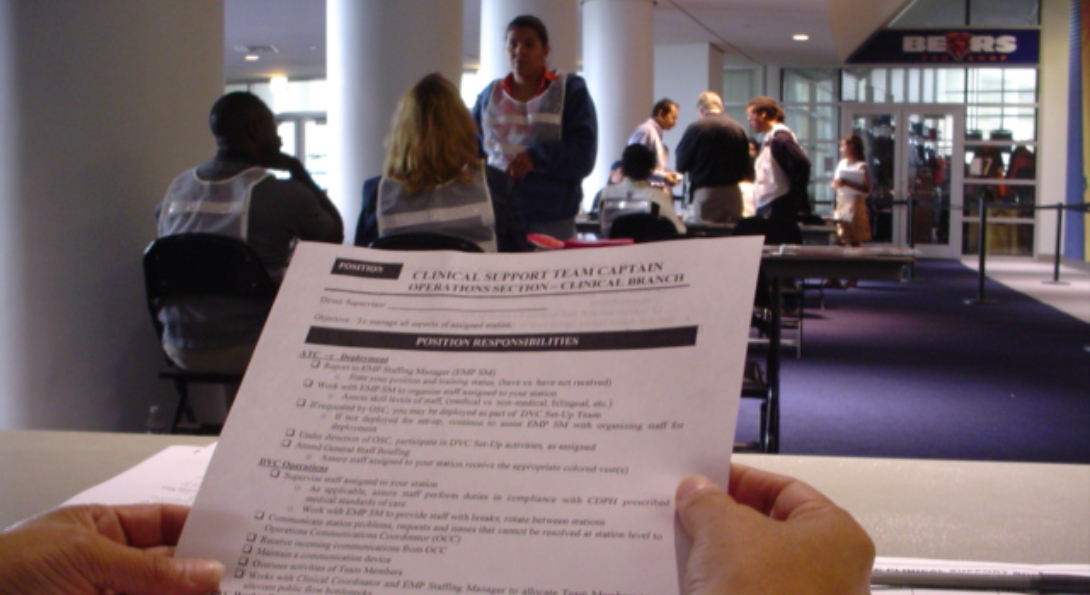
In partnership with the Chicago Department of Public Health and the Center for the Advancement of Distance Education at UIC, we developed an online training simulation on vaccinations, examining steps to vaccinate on a mass scale and determine the number of vaccinations needed to stem the tide of an infectious disease. We worked to develop plans and support full scale exercises such as ones at Soldier Field for the city and local schools for the county.
The Center at UIC was formed before the September 11, 2001 terrorist attacks, and not surprisingly, emphasis on preparedness grew following the disaster. The Center worked with public health agencies in the state on bioterrorism preparation and designed 60 plus courses aligned with public health competencies that became the foundation for the Public Health Emergency Preparedness certificate program at the School.
After Hurricane Katrina, the Center collaborated with the city on preparedness for natural disasters, mainly winter weather events. The project built capacity with first responders to train community members on preparedness kits and building preparedness response plans.
IPHPC worked with the UIC Emergency Management Committee to organize and provide staff support to complete the College and University Pandemic Influenza Planning Checklist. This work led to the development of the Office of Preparedness & Response led by David Ibrahim, PhD, clinical assistant professor of EOHS.
“Everyone considers when an emergency happens that it’s all about money and it’s all about time,” Kapadia said. “There are other factors that we do have control over and can try to have control over.”
As she reflects on the pandemic that has unfolded across the country, Kapadia notes preparation efforts haven’t been perfect. Basic tools such as testing, contact tracing and surveillance are yet to come fully online and data collection is not centralized.
“Everyone keeps saying, ‘We all are in this together,’ and I think looking back at Katrina and other localized disasters, these things do impact all of us,” Kapadia said. “We all have a role to play, and you can’t minimize that each of our actions impacts others.”